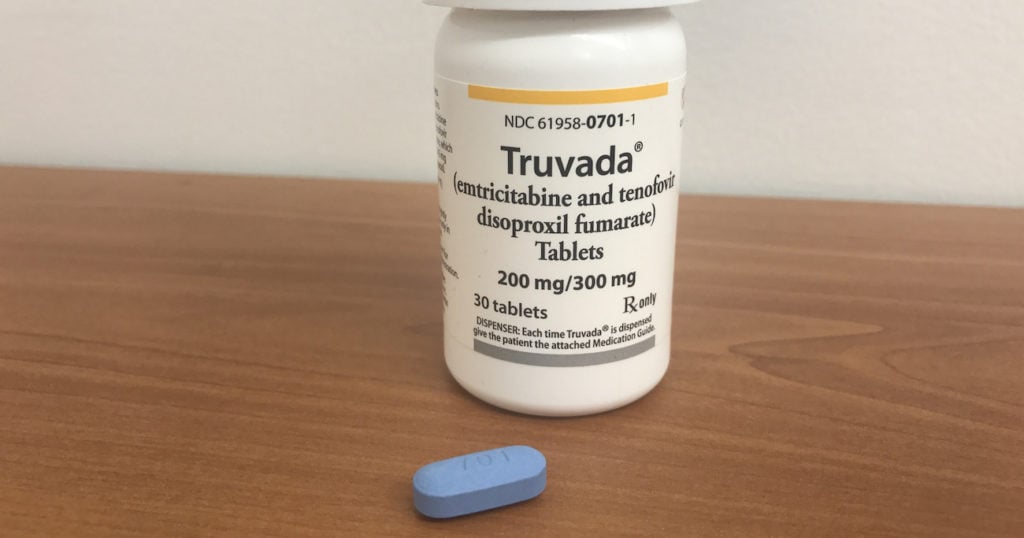
Truvada, or PrEP, is a medication that can reduce HIV infection by more than 90 percent. Health officials consider it an important HIV prevention tool. Democrats in the U.S. House of Representatives and the Senate have collaborated to reintroduce the PrEP Access and Coverage Act of 2023 to help reduce HIV. One of the things that needs to be talked about is that many older people are living with HIV or are at risk of contracting the virus. In 2021, the latest year for which data is available, people over age 50 accounted for 53 percent of people living with HIV in the U.S. By 2030, that proportion may be as high as 70 percent. Also, contrary to stereotype, older people are sexual beings and therefore engage in sexual and other behaviors that put them at risk for the virus infection. In 2021, people 50 and older accounted for 16.4 percent of new HIV diagnoses among those aged 13 and older. Photo: Gilead Sciences.
There was a time when the terms “HIV” and “aging” didn’t go together at all. Now, as effective treatments give people living with HIV a normal life expectancy, those terms do — but aging with HIV raises its own set of issues.
National HIV/AIDS and Aging Awareness Day was Sept. 18, but these issues should be addressed year around.
Some HIV specialists lack knowledge about the health consequences of aging, and specialists in aging often aren’t well-versed regarding the virus.
Medical providers sometimes aren’t aware of how HIV drugs interact with those prescribed for diseases that come with age.
“We’re a little siloed, and we really need to be talking with each other,” says Terri Wilder, HIV/aging policy advocate at SAGE: Advocacy and Services for LGBTQ+ Elders.
One of the things that needs to be talked about is that many older people are living with HIV or are at risk of contracting the virus. In 2021, the latest year for which data is available, people over age 50 accounted for 53 percent of people living with HIV in the U.S. By 2030, that proportion may be as high as 70 percent.
That’s partly due to advances in treatment since the mid-1990s. People who are diagnosed with HIV soon after they are infected, have good access to health care, and start antiretroviral treatment promptly and adhere to it can expect to live as long as people who don’t have the virus.
Also, contrary to stereotype, older people are sexual beings and therefore engage in sexual and other behaviors that put them at risk for HIV infection. In 2021, people 50 and older accounted for 16.4 percent of new HIV diagnoses among those aged 13 and older.
“We just have these blocks in our heads and our vision about who has sex in our society, who uses drugs, who has vulnerabilities,” Wilder says.
But many older people aren’t routinely offered HIV testing. The current guideline from the Centers for Disease Control and Prevention is that medical providers should offer HIV testing on a routine basis to people aged 13 to 64. (Routine, in this case, means unrelated to the patient’s risk profile.) SAGE and organizations it has partnered with in the HIV and Aging Policy Action Coalition, such as the U.S. People Living With HIV Caucus, want to see that upper limit lifted.
“People 65 and over should also be tested routinely,” says Ronald Johnson, a longtime HIV activist and chair of the People Living With HIV Caucus.
SAGE has had several listening sessions with older people living with HIV and found that many were not offered routine testing, and when they did get tested, they had more advanced disease, Wilder says. One spoke of a friend who wasn’t tested until they were hospitalized, then tested positive, and died three weeks later, she says.
“These policies really have life and death consequences,” Wilder points out.
Some states are making progress in this regard. New York State, for instance, has enacted a law lifting the upper limit for routine testing, she notes.
After test results come back, people who test positive should be offered treatment immediately, and those who test negative should be offered pre-exposure prophylaxis (PrEP) or, if they’ve been exposed to the virus but not infected, post-exposure prophylaxis (PeP), Wilder says. She adds that the CDC hasn’t updated its testing guidelines since 2006, so there was no update after Truvada became the first drug approved for PrEP in 2012.
There’s also the question of shared knowledge about HIV and other health conditions. Johnson, a Black gay man who was diagnosed with HIV in 1989, initially didn’t expect to live past 50. Now he’s in his 70s and is in treatment not only for HIV but for cardiovascular issues and more.
“I take about nine prescribed drugs, only one of which is for HIV,” he says. Medical providers treating HIV need to be knowledgeable about the health issues that come with age, and those who treat older patients for those issues need to understand HIV, he says. This includes how the various conditions interact, how the drugs used to treat them do, and the possibility that people with HIV may develop the conditions of age earlier than others. “Those are the kinds of issues that our health care providers across the system need to be aware of,” he says.
Johnson himself is in a good position. “I’m fortunate that my primary physician is very knowledgeable about HIV,” he says. But many people with HIV are not that fortunate.
In addition, there remains outright discrimination against people living with HIV and LGBTQ+ people. This includes discrimination in long-term care, assisted living, and other services needed by older Americans. “It’s not as bad as it was, but it is still happening,” Wilder says.
A few years ago, six nursing homes in Nebraska turned away a man who was living with HIV and dementia. His daughter was finally able to find a facility that would admit him, farther from her home than the others, but he received excellent care there. The American Civil Liberties Union’s Nebraska affiliate issued letters of warning to the homes that had refused to admit him.
SAGE and its coalition partners are pushing an LGBTQ+/HIV Long-Term Care Bill of Rights to protect against this discrimination. A few states, including California and New Jersey, and cities, including San Francisco and Washington, D.C., have enacted such measures, and activists are preparing to introduce one at the national level.
There is also an effort to assure that the Older Americans Act, up for reauthorization by Congress next year, takes note of the special needs of HIV-positive and LGBTQ+ people, Wilder says.
If organizations that receive funding under the act have expertise in serving people with HIV, they should make the public aware, and other groups that serve older people should seek out this expertise, perhaps partnering with HIV groups, she says.
Other services needed include moves to address the isolation and loneliness that older people who are HIV-positive often experience. Additional funding for mental health and the hiring of peer counselors would be enormously helpful, Wilder notes. “There’s nothing like talking with somebody else who has a similar lived experience,” she says.
Johnson encourages older people living with HIV to volunteer with groups serving their population and to speak up about the issues facing them. “We need to be visible,” he says. “We need to be able to say that we are part of the community.”
This article originally appeared on Advocate.com, and is shared here as part of an LGBTQ+ community exchange between Q Voice News and Equal Pride.
